Headaches - cluster
Highlights
What Are Cluster Headaches?
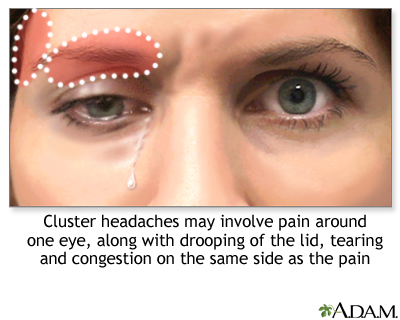
Cluster headaches are among the most painful types of headaches. They are marked by excruciating stabbing and penetrating pain, which is usually centered around the eye. Cluster headache attacks occur very suddenly and without warning, with the pain peaking within 15 minutes.
Symptoms of Cluster Headache Attacks
In addition to pain, symptoms of cluster headaches may include:
- Swollen or droopy eyelid
- Watery, tearing eye
- Stuffy or runny nose
- Contracted eye pupil
- Forehead and facial sweating
- Intolerance to light and sound
Who Gets Cluster Headaches?
- Cluster headaches are rare, affecting less than 1% of the population.
- Men are much more likely to suffer from cluster headaches than women.
- Many people who have cluster headaches have a personal or family history of migraine headaches.
Treatment
Treatment of cluster headaches focuses on relieving pain when attacks occur, and on preventive strategies to reduce attack duration and frequency. Oxygen therapy and sumatriptan (Imitrex, generic) injection are the most effective treatments for acute attacks. Verapamil (Calan, generic), a high blood pressure drug, is typically the first choice of medication used for long-term prevention.
Behavioral treatments can be a helpful supplement to drug therapy. These treatments include relaxation therapy, biofeedback, cognitive-behavioral therapy, and stress management. Patients should also identify and avoid any triggers, such as alcohol use and cigarette smoking, which may provoke cluster headache attacks.
Survey of Cluster Headache Patients
Results from the U.S. Cluster Headache Survey, the largest study of cluster headache patients ever completed in the United States, reveal:
- Diagnostic delays. Many patients with cluster headache experience at least a 5-year delay in having their symptoms correctly diagnosed as cluster headache. Only 21% of survey respondents reported a correct initial diagnosis. Sinusitis and migraine were common misdiagnoses.
- Suicidal thoughts. More than half (55%) of respondents reported experiencing suicidal thoughts.
- Time of attacks. Most cluster headache attacks occur between early evening and early morning hours, with a peak time of midnight - 3 a.m.
- Triggers. Alcohol, especially beer, is the most common trigger of attacks, followed by weather changes and smells.
Introduction
Cluster headaches are among the most painful, and least common, of all headaches. The pain can be so excruciating that they are sometimes referred to as "suicide headaches." Their signature is a pattern of periodic cycles ("clusters") of headache attacks, which may be either:
- Episodic. Attacks occur regularly for 1 week to 1 year, separated by long pain-free periods that last at least 1 month. Between 80 - 90% of patients have episodic cycles. A significant number of people who experience a first cluster attack do not have another one.
- Chronic. Attacks occur regularly for more than 1 year, with pain-free periods lasting less than 1 month. Between 10 - 20% of patients have chronic cluster headaches. The chronic form is very difficult to treat.
Typical Cluster Cycles
Timing of an Attack. Cluster headache attacks tend to occur with great regularity at the same time of day. (For this reason, cluster headaches are sometimes referred to as "alarm clock" headaches.) Most attacks occur between early evening and early morning, with peak time of midnight - 3 a.m.
Duration of an Attack. A single cluster attack is usually brief but extremely painful, lasting about 15 minutes - 1.5 hours if left untreated.
Number of Attacks per Day. During an active cycle, people can experience as few as 1 attack every other day to as many as 8 attacks a day.
Duration of Cycles. Attack cycles typically last 6 - 12 weeks with remissions lasting up to 1 year. In the chronic form, attacks are ongoing, and there is little remission. Attacks cycles tend to occur seasonally, most often in the spring and autumn.
Primary Headaches That Resemble Cluster Headaches
Cluster headaches are a type of primary headache. A headache is considered primary when it is not caused by another disease or medical condition. Other primary headaches that resemble cluster headache include:
- Chronic Paroxysmal Hemicrania. Chronic paroxysmal hemicrania is very similar to cluster headache. It causes multiple, short, and severe daily headaches with symptoms resembling those of cluster headache. As compared to cluster headaches, the attacks are shorter (1 - 2 minutes) and more frequent (occurring an average of 15 times a day). This headache is even rarer than cluster headache, tends to occur in women, and responds to treatment with the anti-inflammatory drug indomethacin (Indocin, generic).
- Hemicrania Continua. Hemicrania continua occurs mostly in women. The pain, which can range from mild to severe, occurs continuously on one side of the face. Periodic attacks can last from days to weeks, and may resemble migraines. It is usually treated with indomethacin.
- SUNCT Syndrome. SUNCT syndrome (short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing) causes stabbing or burning eye pain that may resemble cluster headaches, but attacks are very brief (lasting about a minute) and may occur more than 100 times per day. Red and watery eyes, sweating forehead, and congestion are typical. This rare headache is more common in men than women and does not respond to usual headache treatments.
Causes
Cluster headaches, like migraines, are likely due to an interaction of abnormalities in the blood vessels and nerves that affect regions in the face.
Abnormalities in the Hypothalamus
Evidence strongly suggests that abnormalities in the hypothalamus, a complex structure located deep in the brain, play a major role in cluster headaches. Advanced imaging techniques have shown that a specific area in the hypothalamus is activated during a cluster headache attack.
The hypothalamus is involved in the regulation of many important chemicals and nerve pathways, including:
- Nerve clusters that regulate the body's biologic rhythms (its circadian rhythms)
- Serotonin and norepinephrine. These are neurotransmitters (chemical messengers in the brain) that are involved with well-being and appetite.
- Cortisol (stress hormones)
- Melatonin (a hormone related to the body's response to light and dark)
- Beta-endorphins (substances that modulate pain)
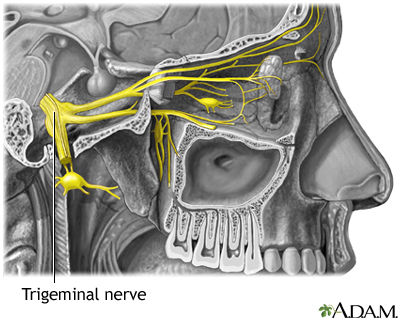
By some not completely understood mechanism, the trigeminal nerve is also involved. The trigeminal nerve carries sensations from the face to the brain.
Circadian Abnormalities. Cluster attacks often occur during specific sleep stages. They also often follow the seasonal increase in warmth and light. Many patients report an increase in attacks when daylight savings time changes occur in the fall and spring. Researchers have therefore focused attention on circadian rhythms, and in particular small clusters of nerves in the hypothalamus that act like biologic clocks. The hormone melatonin is also involved in the body's biologic rhythms.
Dilation of Blood Vessels
Cluster headaches are associated with dilation (widening) of blood vessels and inflammation of nerves behind the eye.
What causes these events and how they relate to cluster headaches are still unclear. Because blood vessel dilation appears to follow, not precede, the pain, some action originating in the brain is likely to be part of the process.
Abnormalities in the Sympathetic Nervous System
Some evidence suggests that abnormalities in the sympathetic (also called autonomic) nervous system may contribute to cluster headaches. This system regulates non-voluntary muscle actions in the body, such as in the heart and blood vessels.
Prognosis
The pain of cluster headaches can be intolerable. In fact, a higher-than-average rate of suicidal thoughts has been reported in men with these headaches. Eventually, as people age, the attacks cease, but doctors cannot predict when or how they will end.
Effects on Mental and Emotional Functioning
Anxiety and depression are common among people with cluster headaches, which can affect functioning and quality of life.
Auras and Medical Risks
Some patients with cluster headaches experience migraine-like aura. Research suggests that headaches that are accompanied by aura may increase the risk of stroke or transient ischemic attack (TIA). TIA symptoms are similar to those of stroke, but last only briefly. A TIA is often a warning sign that a person is at risk for having a more severe stroke. Headaches with auras may also increase the risk for eye retinal damage (retinopathy). Aura-related headaches may affect the small blood vessels in the brain and the eyes, thereby increasing the risks for stroke and retinopathy.
Risk Factors
Cluster headaches are rare, affecting less than 1% of the population.
Age and Gender
Cluster headaches can affect all ages, from children to the elderly, but are most common from young adulthood through middle age. Men are 2 - 3 times more likely to have cluster headaches than women, with the peak age of onset occurring during their 40s. In women, age of onset tends to be in the 60s.
Unlike with migraines, fluctuations in estrogen and other female hormones do not appear play a role in cluster headaches.
Lifestyle Factors
Lifestyle factors, including smoking, alcohol abuse, and stress (in particular stressful work situations), definitely affect cluster headaches. Smoking can trigger attacks. (However, quitting smoking generally does not stop the headaches.) Alcohol, especially beer, is the most common attack trigger.
Family History and Genetic Factors
Cluster headaches tend to run in families, suggesting a genetic component may be involved in some cases.
History of Migraine
About half of people with cluster headache have a personal or family history of migraine. About 15% of patients have both kinds of headache.
Head Injury
Head injury with brain concussion appears to increase the risk of cluster headaches, although a causal relationship has not been proven.
Sleep Apnea and Other Sleep Disorders
Cluster headaches tend to occur during specific sleep stages and have been associated with several sleep disorders, including narcolepsy, insomnia, restless legs syndrome, and sleep apnea.
Sleep apnea, a disorder in which a person's breathing pauses during the night, perhaps hundreds of times, is of particular interest. In some people, apnea may trigger a cluster headache during the first few hours of sleep, making patients susceptible to follow-up attacks during the following midday to afternoon periods. Treating patients who have both disorders with a device called CPAP, which opens the airways, may help improve both conditions. [For more information, see In-Depth Report #65: Sleep apnea.]
Cluster Headache Triggers
The following conditions and substances may trigger cluster attacks:
- Alcohol and cigarette smoking
- Weather changes
- High altitudes (trekking, air travel)
- Smells
- Bright light (including sunlight or flashing lights)
- Exertion
- Heat (hot weather, hot baths or showers)
- Foods high in nitrites (such as bacon and preserved meats)
- Certain medications (including those that cause blood vessel dilation, such as nitroglycerin, and various blood pressure medications)
- Cocaine
Triggers usually have an effect only during active cluster cycles. When the disorder is in remission, such triggers rarely set off the headaches.
Symptoms
Cluster headaches usually strike suddenly and without warning, although some people have a migraine-type aura before the attack. The pain is deep, constant, boring, piercing, or burning in nature, and located in, behind, or around the eye. The pain then spreads to the forehead, jaw, upper teeth, temples, nostrils, shoulder or neck. The pain and other symptoms usually remain on one side of the head.
The pain generally reaches very severe levels within 15 minutes. Patients may feel agitated or restless during an attack and often want to isolate themselves and then move around. Gastrointestinal symptoms are not very common.
Other typical symptoms include:
- Swollen or droopy eyelid
- Watery, tearing eye
- Contraction of the eye pupil
- Stuffy or runny nose
- Forehead and facial sweating
- Restlessness and agitation
- Nausea and vomiting
- Intolerance to light and sound
Diagnosis
Many patients report a delay of more than 5 years in the diagnosis of their cluster headaches. Migraine-like symptoms (light and sound sensitivity, aura, nausea, vomiting) are major reasons for the frequent misdiagnosis. In some cases, patients are inappropriately treated for other types of headaches (like migraine) or health conditions (like sinusitis).
Medical and Personal History
Cluster headache is diagnosed by medical history, including the pattern of recurrent attacks, and by typical symptoms (swollen eyelid, watery eye, runny nose). Keeping a headache diary to record a description of attacks can help the doctor make an accurate diagnosis. The patient should describe to the doctor:
- Frequency of attacks (if keeping a diary, record the date and time of each attack)
- Description of pain (stabbing, throbbing)
- Location of pain
- Duration of pain
- Intensity of pain (using a number scale like the one below)
- Associated symptoms (tearing eyes, nausea and vomiting, sweating)
- Any measures that bring relief (applying pressure, going out for fresh air)
- Any events that preceded or may have triggered the attack
- Any medications you are taking
- Behaviors during a headache (restlessness, agitation)
- Snoring, sleep disturbances, or daytime sleepiness (these could relate to sleep apnea, which is sometimes associated with cluster headache)
Pain may be indicated by using a number system:
1 = Mild, barely noticeable
2 = Noticeable, but does not interfere with work or activities
3 = Distracts from work or activities
4 = Makes work or activities very difficult
5 = Incapacitating
Physical Examination
To diagnose a chronic headache, the doctor will examine the head and neck and perform a neurologic examination, which includes a series of simple exercises to test strength, reflexes, coordination, and sensation. The doctor may also examine the eyes. The doctor may ask questions to test short-term memory and related aspects of mental function.
Imaging Tests
The doctor may order a computed tomography (CT) scan or magnetic resonance imaging (MRI) test of the head to check for brain abnormalities that may be causing the headaches.
Ruling Out Other Headaches and Medical Disorders
As part of the diagnosis, a doctor should rule out other headaches and disorders. If the results of the history and physical examination suggest other or accompanying causes of headaches or serious complications, extensive imaging tests are performed.
Migraines. Cluster headaches are often misdiagnosed as migraines but they are quite different:
- Frequency and Duration. Cluster headaches generally last 15 minutes to a few hours and can occur several times a day. A single migraine attack is continuous over the course of one or several days.
- Behavior. Cluster headache sufferers tend to move about while migraine sufferers usually want to lie down.
Nevertheless, in both cases, the headache suffers can be highly sensitive to light and noise, which may make it difficult to distinguish between them.
Other Headaches. Other headaches that resemble migraines include SUNCT (short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing) and chronic paroxysmal hemicrania, which are other primary headaches, and some secondary headaches notably trigeminal neuralgia (TN), temporal arteritis, and sinus headaches. Cluster symptoms, however, are usually precise enough to rule out these other types of headaches.
Tear in the Carotid Artery. A tear in the carotid artery (which carries blood to the brain) can cause pain that resembles a cluster headache. People with this condition may even respond to sumatriptan, a drug used to treat a cluster attack. Doctors should consider imaging tests for patients with a first episode of cluster headache in which this event is suspected.
Orbital Myositis. An unusual condition called orbital myositis, which produces swelling of the muscles around the eye, may mimic symptoms of cluster headache. This condition should be considered in patients who have unusual symptoms such as protrusion of the eyeball, painful eye movements, or pain that does not dissipate within 3 hours.
Headache Symptoms that Could Indicate Serious Underlying Disorders
Headaches indicating a serious underlying problem, such as cerebrovascular disorder or malignant hypertension, are uncommon. (It should be emphasized that a headache is not a common symptom of a brain tumor.) People with existing chronic headaches, however, might miss a more serious condition believing it to be one of their usual headaches. Such patients should immediately call a doctor if the quality of a headache or accompanying symptoms has changed. Everyone should call a doctor for any of the following symptoms:
- Sudden, severe headache that persists or increases in intensity over the following hours, sometimes accompanied by nausea, vomiting, or altered mental states (possible indication of hemorrhagic stroke, which is also called brain hemorrhage).
- Sudden, very severe headache, worse than any headache ever experienced (possible indication of brain hemorrhage or a ruptured aneurysm).
- Chronic or severe headaches that begin after age 50.
- Headaches accompanied by other symptoms, such as memory loss, confusion, loss of balance, changes in speech or vision, or loss of strength in or numbness or tingling in arms or legs (possibility of small stroke in the base of the brain).
- Headaches after head injury, especially if drowsiness or nausea are present (possibility of brain hemorrhage).
- Headaches accompanied by fever, stiff neck, nausea and vomiting (possibility of spinal meningitis).
- Headaches that increase with coughing or straining (possibility of brain swelling).
- A throbbing pain around or behind the eyes or in the forehead accompanied by redness in the eye and perceptions of halos or rings around lights (possibility of acute glaucoma).
- A one-sided headache in the temple in elderly people; the artery in the temple is firm and knotty and has no pulse; scalp is tender (possibility of temporal arteritis, which can cause blindness or stroke if not treated).
- Sudden onset and then persistent, throbbing pain around the eye possibly spreading to the ear or neck unrelieved by pain medication (possibility of blood clot in one of the sinus veins of the brain).
Managing Cluster Headaches
Management of cluster headaches focuses on:
- Acute therapy for stopping an attack while it is happening
- Preventive therapy for stopping or reducing attack recurrences
Treating Attacks
The most effective and best-studied treatments for a cluster attack are:
- Oxygen inhalation.
- Triptan drugs. Usually an injection of the triptan drug sumatriptan (Imitrex, generic), which is FDA-approved for cluster headache treatment. Intranasal formulations of sumatriptan or zolmitriptan (Zomig) are alternatives.
Relief can occur in 5 - 10 minutes. Oxygen and sumatriptan injection are sometimes given together.
Other drugs that may be used for acute attacks are nasal sprays of dihydroergotamine or lidocaine.
Preventing Attacks
Cluster headache attacks are usually short, lasting from 15 - 180 minutes, and the excruciating pain may have subsided by the time a patient reaches a doctor’s office or emergency room.
Because it can be difficult to treat attacks when they occur, treatment efforts focus on the prevention of attacks during cluster cycles. Although certain drugs are standard, preventive therapy needs to be individually tailored for each patient. The doctor may prescribe a combination of drugs.
Verapamil (Calan, generic), a calcium-channel blocker drug, is the mainstay preventive treatment for cluster headaches. However, it can take 2 - 3 weeks for this drug to take effect. During this period, corticosteroids (typically prednisone) may be used as an initial transitional therapy. For long-term treatment of chronic cluster headaches, lithium may be used as an alternative to verapamil.
Although they are not FDA-approved for cluster headache, anti-seizure drugs such as divalproex sodium (Depakote, generic) valproate sodium (Depacon, generic), valproic acid (Depakene, generic), topiramate (Topamax, generic), and gabapentin (Neurontin) are sometimes used for preventive treatment.
Behavioral Treatments and Lifestyle Changes
Behavioral Treatments. Behavioral therapies are a helpful accompaniment to drug treatment. These approaches can help with pain management and enable patients to feel more in control of their condition.
Behavioral approaches include:
- Relaxation treatment combined with biofeedback
- Cognitive-behavioral therapy
Lifestyle Changes. Patients should avoid the following triggers that may provoke cluster headache attacks:
- Alcohol. Heavy alcohol use is strongly associated with cluster headaches, although it is not clear if alcohol triggers pain or is simply used as a coping mechanism for dealing with severe pain.
- Cigarette smoking. Many studies indicate that a majority of patients with cluster headache are cigarette smokers. While studies have not shown that quitting cigarettes will stop cluster headaches, smoking cessation should still be a goal. Smokers who can't quit should at least stop at the first sign of an attack and not smoke throughout a cycle.
Treatment for Acute Attacks
Oxygen Therapy
Breathing pure oxygen (by face mask, for 15 minutes or less) is one of the most effective and safest treatments for cluster headache attacks. It is often the first choice treatment. Inhalation of oxygen raises blood oxygen levels, therefore relaxing narrowed blood vessels.
Triptans
Triptans are drugs that are usually used to treat migraine headaches. They can also help stop a cluster attack. An Injection of sumatriptan (Imitrex, generic) is the standard triptan treatment and is FDA-approved for cluster headaches. Sumatriptan injections usually work within 15 minutes. The nasal spray form may also be effective for some patients, and generally provides relief within 30 minutes. The spray seems to work best for attacks that last at least 45 minutes, although some people find it does not work as well as the injectable form.
Zolmitriptan (Zomig) is another triptan drug used for cluster headache treatment. It is given in either oral or nasal spray form. Zolmitriptan may have fewer side effects than sumatriptan.
Side Effects. Side effects of sumatriptan may include:
- Nausea
- Dizziness
- Muscle weakness
- Heaviness or pressure in the chest
- Tingling and numbness in the toes
- Rapid heart rate
Complications and Contraindications of Triptans. The following are potentially serious problems with triptans:
- Complications on the Heart and Circulation. Triptans narrow (constrict) blood vessels. Because of this action, spasms in the blood vessels may occur, which can cause stroke and heart attack. This is a rare but very serious side effect. Patients with a history of heart attack, stroke, angina, uncontrolled high blood pressure, peripheral artery disease, or heart disease should not use triptan drugs.
- Serotonin Syndrome. Serotonin syndrome is a life-threatening condition that occurs from an excess of the brain chemical serotonin. Triptans, as well as certain types of antidepressant medications, can increase serotonin levels. These antidepressant drugs include serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac, generic), paroxetine (Paxil, generic), and sertraline (Zoloft, generic) and selective serotonin/norepinephrine reuptake inhibitors (SNRIs) such as duloxetine (Cymbalta) and venlafaxine (Effexor, generic). It is very important that patients not combine a triptan drug with an SSRI or SNRI drug. Serotonin syndrome is most likely to occur when starting or increasing the dose of a triptan or antidepressant drug. Symptoms include restlessness, hallucinations, rapid heartbeat, tremors, increased body temperature, diarrhea, nausea, and vomiting. You should seek immediate medical care if you have these symptoms.
Ergotamine
Injections of the ergotamine-derived drug known as dihydroergotamine (DHE, Migranal) can stop cluster attacks within 5 minutes in many patients, offering benefits similar to injectable sumatriptan. Ergotamine is also available in the form of a nasal spray, rectal suppositories, and tablets.
Ergotamine can have dangerous drug interactions with many medications, including sumatriptan. All ergotamine products approved by the Food and Drug Administration (FDA) contain a "black box" warning in the prescription label explaining these drug interactions. Because ergotamine constricts blood vessels, patients with peripheral vascular disease should not use this drug.
Local Anesthetics
Lidocaine, a local anesthetic, may be useful in nasal-spray or nasal-drop form for stopping cluster attacks. It usually takes effect within about 40 minutes. Lidocaine can have an unpleasant taste. Some doctors recommend that patients try a nasal application of lidocaine to see if it helps ease pain.
Capsaicin is a compound derived from hot pepper. Some patients who have not found relief through other medications use it to treat or prevent cluster headaches by applying it intranasally. There have been few studies to confirm its effectiveness. It can cause an intense burning sensation.
Preventive Medications
Calcium-Channel Blockers
Calcium-channel blockers, commonly used to treat high blood pressure and heart disease, are important drugs for preventing episodic and chronic cluster headaches. Verapamil (Calan, generic) is the standard calcium-channel blocker used for cluster headache prevention. It can take 2 - 3 weeks to have a full effect, and a corticosteroid drug may be used in combination during this transitional period. Constipation is a common side effect.
People taking calcium-channel blockers should not stop taking the drug abruptly. Doing so can dangerously increase blood pressure. Overdose can cause dangerously low blood pressure and slow heart beats.
Lithium
Lithium (Eskalith, generic), commonly used for bipolar disorder, may also help prevent cluster headaches. The benefits of lithium usually appear within 2 weeks of starting the drug, and often within the first week. Lithium may be used alone or with other drugs. Lithium can have many side effects including trembling hands, nausea, and increased thirst. Weight gain is a common side effect with long-term use. [For more information, see In-Depth Report #66: Bipolar disorder.]
Corticosteroids
Corticosteroid drugs (also called steroids) are very useful as transitional drugs for stabilizing patients after an attack until a maintenance drug, such as verapamil, begins to take effect. Prednisone (generic) and dexamethasone (Decadron, generic) are the standard steroid drugs used for short-term cluster headache transitional treatment. These drugs are typically taken for a week and then gradually tapered off. If headaches return, the patient may start taking the steroid again. Unfortunately, long-term use of steroids can lead to serious side effects so they cannot be taken for on-going prevention.
Steroid injections may also provide short-term relief. Some patients are helped by an occipital nerve block in which an anesthetic and a corticosteroid are injected into the occipital nerve in the back of the head. Researchers are also investigating suboccipital injections where a steroid is injected into the base of the skull on the same side as the headache attack.
Anti-Seizure Drugs
Anti-seizure drugs, which are used for epilepsy treatment, may be helpful for preventing cluster headaches in some patients. They include older drugs such as divalproex (Depakote, generic), valproate (Depacon, generic), and valproic acid (Depakene, generic) and newer drugs such as topiramate (Topamax, generic) and gabapentin (Neurontin, generic). More research needs to be done to evaluate how effective these drugs are at preventing cluster headaches.
Side Effects. Anti-seizure medication side effects vary by drug but may include:
- Nausea and vomiting
- Diarrhea
- Cramps
- Tingling sensation in arms and legs
- Hair loss
- Dizziness
- Sleepiness
- Blurred vision
- Weight gain (or with topiramate, weight loss)
- Valproate and divalproex can cause serious side effects of inflammation of the pancreas (pancreatitis) and damage to the liver
Valproate products and topiramate can increase the risk for birth defects, particularly cleft palate. These drugs should not be used during the first trimester of pregnancy. Women who are of child-bearing age and considering pregnancy should discuss the safety of these drugs with their doctors and consider other types of migraine preventive medication.
All anti-seizure drugs may increase the risks of suicidal thoughts and behavior (suicidality). The highest risk of suicide can occur as soon as 1 week after beginning drug treatment and can continue for at least 24 weeks. Patients who take these drugs should be monitored for signs of depression, changes in behavior, or suicidality. [For more information, see In-Depth Report #44: Epilepsy.
Investigational Drugs
Botulinum. Botulinum toxin A (Botox) injections are typically used to smooth wrinkles. Botox is also being studied for treatment of headaches, and is approved for prevention of chronic migraine. Research on its use for cluster headache prevention is still preliminary, and there is not sufficient evidence to support its efficacy.
Melatonin. Small reports indicate that melatonin, a brain hormone that helps to regulate the sleep-wake cycle, may help prevent episodic or chronic cluster headaches. Melatonin supplements are sold in health food stores, but as with most natural remedies, the quality of different preparations varies, and they have not been rigorously tested for safety or effectiveness. More studies are needed.
Surgery
In rare cases, surgical intervention may be considered for patients with chronic cluster headaches that do not respond to other treatments. Patients whose headaches have not gone into remission for at least a year may also be candidates for surgery. Most surgical approaches for cluster headache are still considered experimental, having been tested only on a relatively small number of patients. Surgery has shown limited success and can have distressing side effects. However, some surgical techniques, such as deep brain electrical stimulation, are showing promise.
Deep Brain Electrical Stimulation
Deep brain stimulation (also called neurostimulation) may relieve chronic cluster headaches in some patients who do not respond to drug therapy. A similar technique is approved for treating the tremors associated with Parkinson's disease. The surgeon implants a tiny wire in a specific part of the hypothalamus. The wire receives electrical pulses from a small generator implanted under the collarbone.
Although only a small number of patients have been treated, results to date are promising. Some patients have remained completely free of pain for an average of more than 7 months when the electrode is switched on. When the device is turned off, headaches reappear within days to weeks. The procedure is reversible and appears to be generally safe, although a few cases of fatal cerebral hemorrhage have occurred.
Occipital Nerve Stimulation
Occipital nerve stimulation is being investigated as a less invasive and less risky alternative to deep brain hypothalamus stimulation. Recent studies have reported promising results in a small group of patients with cluster headaches. Some patients became pain-free, while others had reduced frequency of headache attacks.
Vagus Nerve Stimulation
The vagus nerve runs between the brain and the abdomen. Vagus nerve stimulation (VNS) is a surgical procedure in which a small generator is placed under the skin on the left side of the chest. A surgeon makes a second incision in the neck and connects a wire from the generator to the vagus nerve. A doctor programs the generator to send mild electrical pulses at regular intervals. These pulses stimulate the vagus nerve.
VNS is sometimes used to treat epilepsy and depression that does not respond to drugs. It is also being investigated as a possible treatment for chronic migraine and cluster headaches.
Procedures to Block or Remove Facial Nerves That Cause Pain
Percutaneous Radiofrequency Retrogasserian Rhizotomy. Percutaneous radiofrequency retrogasserian rhizotomy (PRFR) generates heat to destroy pain-carrying nerve fibers in the face. Unfortunately complications are common and include numbness, weakness during chewing, changes in tearing and salivation, and facial pain. In severe, but rare, cases, complications include damage to the cornea and vision loss.
Percutaneous Retrogasserian Glycerol Rhizolysis. Percutaneous retrogasserian glycerol rhizolysis (PRGR) is a less invasive technique than PRFR and has fewer complications. It involves injections of glycerol to block the facial nerves that cause the pain. Cluster headaches usually recur.
Microvascular Decompression of the Trigeminal Nerve. Microvascular decompression frees the trigeminal nerve from any blood vessels that are pressing against it. The procedure is risky, and possible complications include nerve and blood vessel injury and spinal fluid leakage. There is reasonably good evidence that it is not effective for treatment of cluster headaches.
Resources
- www.headaches.org -- National Headache Foundation
- www.achenet.org -- American Headache Society
- www.painfoundation.org -- National Pain Foundation
- www.ouch-us.org -- Organization for Understanding Cluster Headaches
References
Ashkenazi A, Schwedt T. Cluster headache--acute and prophylactic therapy. Headache. 2011 Feb;51(2):272-86. doi: 10.1111/j.1526-4610.2010.01830.x.
Barloese M, Jennum P, Knudsen S, Jensen R. Cluster headache and sleep, is there a connection? A review. Cephalalgia. 2012 Apr;32(6):481-91. Epub 2012 Mar 9.
Bartsch T, Paemeleire K, Goadsby PJ. Neurostimulation approaches to primary headache disorders. Curr Opin Neurol. 2009 Jun;22(3):262-8.
Cohen AS, Burns B, Goadsby PJ. High-flow oxygen for treatment of cluster headache: a randomized trial. JAMA. 2009 Dec 9;302(22):2451-7.
Grover PJ, Pereira EA, Green AL, Brittain JS, Owen SL, Schweder P, et al. Deep brain stimulation for cluster headache. J Clin Neurosci. 2009 Jul;16(7):861-6. Epub 2009 Apr 23.
Hedlund C, Rapoport AM, Dodick DW, Goadsby PJ. Zolmitriptan nasal spray in the acute treatment of cluster headache: a meta-analysis of two studies. Headache. 2009 Oct;49(9):1315-23.
Law S, Derry S, Moore RA. Triptans for acute cluster headache. Cochrane Database Syst Rev. 2010 Apr 14;4:CD008042.
Leone M, Bussone G. Pathophysiology of trigeminal autonomic cephalalgias. Lancet Neurol. 2009 Aug;8(8):755-64.
Leroux E, Valade D, Taifas I, Vicaut E, Chagnon M, Roos C, et al. Suboccipital steroid injections for transitional treatment of patients with more than two cluster headache attacks per day: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2011 Oct;10(10):891-7. Epub 2011 Sep 6.
Nesbitt AD, Goadsby PJ. Cluster headache. BMJ. 2012 Apr 11;344:e2407. doi: 10.1136/bmj.e2407.
Rozen TD, Fishman RS. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache. 2012 Jan;52(1):99-113. doi: 10.1111/j.1526-4610.2011.02028.x. Epub 2011 Nov 11.
Schurks M, Kurth T, de Jesus J, Jonjic M, Rosskopf D, Diener HC. Cluster headache: clinical presentation, lifestyle features, and medical treatment. Headache. 2006 Sep;46(8):1246-54.
Tyagi A, Matharu M. Evidence base for the medical treatments used in cluster headache. Curr Pain Headache Rep. 2009 Apr;13(2):168-78.
|
Review Date:
12/17/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |


